NOTE: This blog is the opinion of the author, Rosie Filling, and not of Endo
As a seasoned professional in the pharmaceutical industry, I have long been passionate about developing innovative treatments that improve patients’ lives. However, my understanding of clinical research took on a new dimension in August 2020 when I was diagnosed with cancer and decided to participate in a clinical trial.
This unexpected turn of events (during the COVID-19 crisis) quickly transformed me from a drug development expert to a concerned patient navigating the complex world of healthcare. There are so many different aspects of this life-altering experience I would like to discuss. But for the purposes of this blog, I will highlight the critical importance of aligning the clinical trial technologies patients are asked to use – with their actual needs, capabilities, and lifestyles.
The Informed Consent Process
At my initial appointment, after verbally agreeing to participate in a study, I was presented with an overwhelming amount of information and treatment options that left me feeling vulnerable and uncertain. Despite my extensive knowledge in the field, considering trial participation while coming to terms with my diagnosis was a daunting task. However, my commitment to advancing medical care, my desire to give back, and the reassurance of my support network kept me moving forward.
By leveraging innovative technologies while maintaining a steadfast commitment to patient and site perspectives, we can optimize data collection to ultimately accelerate the development of life-changing treatments.
Even with my industry background, I found the informed consent process to be overwhelming because of the volume of paper forms filled with medical jargon and legal terms. Trying to absorb this complex information during such a confusing and frightening time was tough. I couldn’t help but imagine how difficult it would be for someone with no healthcare background and limited or no support system. I managed to share PDFs with my support network, but the process was less than convenient. I would have preferred electronic documentation that I could review anytime or anywhere – and easily shared with family, friends, and colleagues who could help me decipher what I was agreeing to.
Completing Diaries: When, Where, and How?
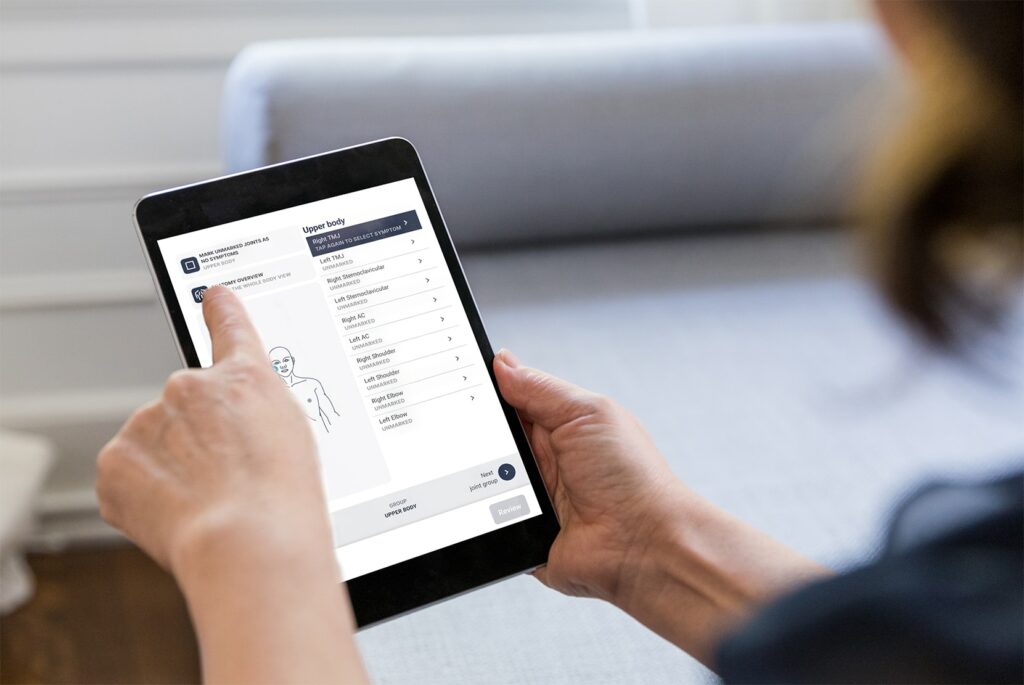
 My study also required me to complete paper diaries. As someone who considers herself fairly tech-savvy, I would’ve been more comfortable with a digital option. However, that’s not the case for everyone, and I believe offering more options and flexibility is the answer. I vividly remember helping an elderly patient with her electronic diary in our shared infusion room. She was on the phone with her granddaughter asking for help with the technology. It really hit home how important it is to design tech tools with patients in mind. Trying to fill out any kind of diary during an infusion is challenging – you’re often feeling unwell, upset, drowsy, and are tangled up in tubes. The site staff did their best to help, but they were juggling so many other tasks – some of them emergency situations.
My study also required me to complete paper diaries. As someone who considers herself fairly tech-savvy, I would’ve been more comfortable with a digital option. However, that’s not the case for everyone, and I believe offering more options and flexibility is the answer. I vividly remember helping an elderly patient with her electronic diary in our shared infusion room. She was on the phone with her granddaughter asking for help with the technology. It really hit home how important it is to design tech tools with patients in mind. Trying to fill out any kind of diary during an infusion is challenging – you’re often feeling unwell, upset, drowsy, and are tangled up in tubes. The site staff did their best to help, but they were juggling so many other tasks – some of them emergency situations.
This experience made me realize how valuable it would be to have patients and site staff involved in designing these technologies. It would be so much easier for patients to complete their diaries at home, between treatments, when they’re feeling better – maybe with help from family. It would ultimately yield more accurate patient-reported data and free up the site staff to focus on patient care and running the trial smoothly.
Making the Most of Connected Devices
Another element of my study was that I was asked to wear a device for remote heart monitoring. Unfortunately, the site staff had not been adequately trained to provide me with the necessary guidance. The device’s placement near my port location caused discomfort and distress, highlighting the importance of centering wearable technology around the patient’s experience. While these devices can be incredibly valuable in collecting vital data, it is crucial that their implementation is accompanied by comprehensive staff training and patient education to ensure a positive experience.
Let’s Keep Making Progress!
My journey, though challenging, has reignited my passion for patient advocacy and deepened my appreciation for the vital role of clinical trial sites. Healthy today, I do my part to ensure that patient and site voices are heard and valued. By leveraging innovative technologies while maintaining a steadfast commitment to patient and site perspectives, we can optimize data collection to ultimately accelerate the development of life-changing treatments. By aligning our efforts with the needs and experiences of those we serve, we can create a brighter, healthier future for all.
For more details on Rosie’s personal oncology clinical trial journey, you may view this on-demand webinar.
To learn more about Rosie’s perspectives on the crucial role of sites in clinical trials, you may watch this video recorded at YPrime’s Innovation Network Gathering.
Check out our other patient engagement resources
about trial design, data capture, operational efficiencies, and, ultimately, solving for certainty in clinical research.